The challenge to combat clinical problems of healthcare acquired infection and worldwide pandemics of COVID, HIV, hepatitis and malaria, to respond to emerging infection problems such as SARS or swine flu and to rationalise antibiotic use in the light of increasing microbial resistance, makes Infectious Diseases an exciting and contemporary specialty.
Infectious Diseases (ID) provides the opportunity of having a career ranging from challenging and constantly varied clinical management, to intellectually stimulating frontier research into diseases of worldwide importance.
The Traditional Backgrounds of ID and Microbiology/Virology
Traditionally, ID was quite distinct from the laboratory based infection specialties: ID physicians had clinical responsibility for patients with mostly communicable diseases; microbiologists/virologists organised and supervised laboratory diagnostic services for infection, led on infection control services, and gave advice to other clinicians about management of various infections, often by telephone, with limited ward reviews.
Changing Specialties
This separation of duties is becoming blurred over time. ID physicians deal with fewer communicable diseases, whilst with technological advances, laboratory supervision is slowly moving over to clinical scientists. The work of ID physicians and microbiologists and virologists has more overlap, particularly in areas of healthcare acquired infection, and antimicrobial resistance.
Combined Infection Training
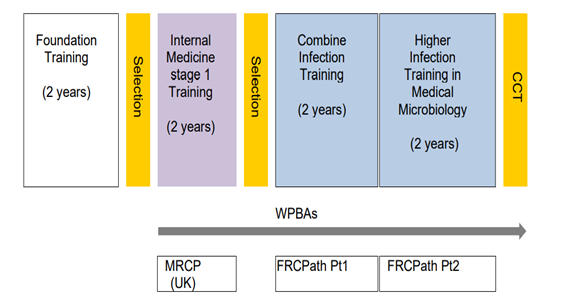
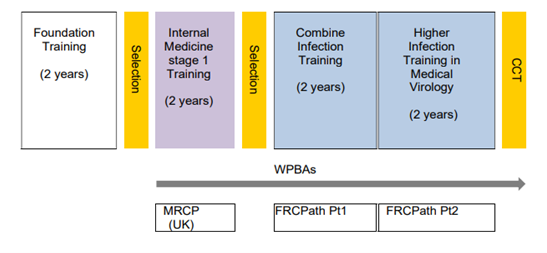
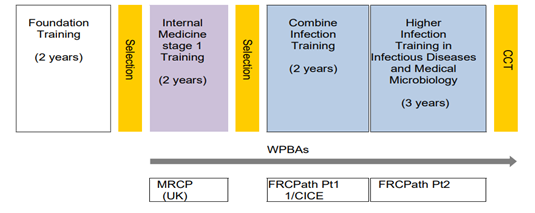
As a result of this change, and looking to the future, August 2015 saw the combined Royal Colleges introduce a new 2 year “combined infection training”(CIT) programme which all trainees in these infection specialties will undertake in their first 2 years of specialty training, before higher specialty training in later years.
Internal Medicine Training (IMT) or Acute Care Common Stem (ACCS) and Membership of the Royal College of Physicians (MRCP) is required for entry into CIT. For further information on IMT, please visit (https://www.imtrecruitment.org.uk/about-imt/about-imt ) and for further information on ACCS, please visit (https://www.imtrecruitment.org.uk/about-imt/about-accs)
The specific entry requirements for combined infection training differ according to the specialty or dual training that is being applied for.
Infection training has five potential training routes (NB. Currently HEEWM only offers joint training pathways ie ID/GIM; ID/MM or ID/MV)
- Medical Microbiology (MM)
- Medical Virology (MV)
- Infectious diseases (ID) with Medical microbiology (ID/MM)
- Infectious Diseases (OD) with Medical Virology (ID/MV)
- Infectious Diseases with General Internal Medicine (GIM) (ID/GIM)
Entry to Medical microbiology or virology or ID/Med Micro or ID/Virology dual training requires:
Two years of Stage 1 Internal Medicine (IMT) plus MRCP(UK)
or
Three years of Acute Care Common Stem –Internal Medicine (ACCS-IM) plus MRCP(UK).
Entry to ID/GIM requires:
Three years of Stage 1 Internal Medicine (IMT) plus MRCP(UK)
Or
Four Years of Acute Care Common Stem- Internal Medicine (ACCS-IM) plus MRCP(UK)
Infection training can also be offered with Academic Clinical Fellowships (ACFs) for those trainees interested to train in academic medicine. ACFs offer trainees to follow an academic route after successfully finishing training. ACFs have an opportunity to do research up to PhD level during their training as part of the preparation for academic career.
The 2021 Curriculum for Specialty Training in Infectious Diseases/Medical Microbiology/Virology
A new curriculum for the infection specialties has been developed and is to be introduced in a staged manner from August 2021. New entrants to CIT in August 2021 training in ID/Micro; ID/virology or mono-specialty micro/virology will commence on the new curriculum. New ID/GIM CIT trainees will commence the new curriculum from August 2022.
Current trainees who are scheduled to obtain CCT on or before August 31st 2023 will remain on the old curriculum. All other trainees will transfer to the new curriculum from August 2022.
- Medical Microbiology (MM) Training Structure 4 years (mono-specialty MM not offered by HEEWM)
- Medical Virology (MV) Training Structure4 years (mono-specialty MV notoffered by HEEWM)
- Infectious Diseases with Medical Microbiology (ID/MM) Training Structure 5 years
- Medical Microbiology with General Internal Medicine (MM/GIM) 5 years
This follows the ID/MM training structure
West Midlands is no longer appointing to mono-specialty microbiology or virology training programmes although such training is still available in some regions.
Why Choose West Midlands for Infection Training?
The West Midlands programme, with approximately 24 infection trainees, is big enough to offer a broad, thorough training and friendly peer support from a good number of fellow trainees, whilst being small enough to support individuals’ specific training aims.
The ID-Micro/Virology/ GIM programmes are well established in the region, and indeed the largest group of infection trainees are now the ID-Medical microbiology arm. We benefit from being a centre for military infectious diseases medicine, including training of military personnel in infection specialties.
The largest ID unit in the West Midlands, and the major ID training centre, is at Birmingham Heartlands Hospital (BHH), which is part of the University Hospitals Birmingham Trust (UHB). The department is long established, vibrant, and expanding -reassuringly so in the current economic climate. All subspecialties are managed or co-managed by the ID consultants. This includes a large in- & out- patient TB service, HIV chronic Hepatitis B&C, bone infection and OPAT services etc.In keeping with the current evolution of infection specialties UHB ID specialists work in an integrated manner with microbiology and virology colleagues across all sites within the Trust. Similar cooperative working is also found at other training sites in the region.
There are 3 other training centres for ID in the region: trainees will oftenspend their first year of infectious diseases training (as part of CIT) at either University Hospital of North Midlands, or Royal Worcester Hospital, or University Hospital of Coventry & Warwickshire. Further years are largely based in BHH but other centres can also accommodate more senior trainees.
Microbiology and virology training takes place across region and trainees benefit from experiencing learning and working in a variety of settings.
Is ID the Job for me?
What can I expect from the Infectious Diseases part of my rotation in West Midlands?
Infectious Diseases is very much a hands-on infection speciality where patient contact is imperative in helping to make the diagnosis. There is a huge variety in the cases that you will see as a Registrar, making your days highly varied, interesting and occasionally exciting. Given this variety, there are a large number of specific areas on which you will be able to focus for possible future research projects and also areas of interest as you progress through your training. As an Infectious Diseases Registrar, you will spend time on the wards, the consult service and in clinics. You don’t have to have travelled or worked abroad to consider a career in Infectious Diseases. You do, however, have to have an interest in organisms as well as people, and will develop a good knowledge of microbiology and how the lab and the processing of samples takes place as part of CIT .
The Infectious Diseases wards can have patients admitted with common infections such as cellulitis and pneumonia, to more unusual cases such as TB (including multi-drug resistant cases), HIV, tropical infections including malaria, leptospirosis, typhoid. The acute and ongoing daily management of such patients is imperative for enhancing your knowledge of Infectious Diseases and the natural history of infections and response to treatments.
The ID teams across the region have been central to the management of patients with COVID19 during the SARS-CoV2 pandemic.
Infection consult services are an ever expanding development n most hospitals given the increasing numbers of complicated surgeries conducted, more immunosuppressive treatments, together with increasing foreign travel, an ageing population and increasing antibiotic resistance rates. The Infectious Diseases team work in an integrated manner with Microbiology when managing such patients, which is essential when determining specimen collection, processing and interpretation of results. The range of problems seen by a typical consult service is vast, ranging from endocarditis, Staphylococcus aureus bacteraemia, bone and joint infections, transplant related infections etc. Your role will involve interaction with various specialities when their patients have an infection issue, providing expertise on the management aiming to aid identification of the source of infection, optimal antibiotic choice and optimal duration of therapy. You will also provide a link to the Outpatient Antimicrobial Therapy (OPAT) services which mst hospitals provide, ensuring prompt discharge of patients who are well enough to be managed in the community.
As part of the consult service, you will link with GPs in the community, providing travel advice, answers to general infection questions and accepting referrals when appropriate.
An example of an interesting case involved a patient being referred to ID, having recently returned from the rainforest of Peru, with cellulitis on her scalp which was not improving following multiple courses of antibiotics. Her GP had reviewed her and thought he saw something moving underneath the skin, and wondered about an infestation. With a small incision and gentle pressure, the botfly larva seen below was removed from the patient’s scalp.

Dermatobiahominis (human botfly)
There are also a range of Infectious Diseases clinics, which you will be able to gain experience in throughout your years of training. These consist of general ID, TB, HIV (with ID and GUM Consultants), Hepatitis (with ID and Gastroenterology Consultants), bone infection and OPAT clinics.
Through the daily review of infection patients, understanding their long-term management and following them up in clinic, you will be provided with excellent first-hand Infectious Diseases experience and knowledge which will form the basis of your continued development in this speciality.
What can I expect from “microbiology” in West Midlands?
The workload is varied: in the morning you may be required to lead the laboratory ‘bench round’ during which new potentially significant isolates are shown to you that require your clinical input. You may then go on a ward round of the intensive care unit and then review ward patients with significant positive cultures. You and ID colleagues will be a key member of several multi-disciplinary team (MDTs) meetings such as infective endocarditis, bone and joint infection, neurosurgical infections, renal transplant, water safety where you will be giving expert microbiology advice on management of complicated infections.
Apart from the MDTs, you will liaise with a variety of people during your time in microbiology: hospital based clinicians, general practitioners, the infection control team, the local public health team and reference laboratories to name but a few.
As a consultant, it is vital to have an understanding of the way results of investigations are derived, so that you can act on results that do not fit the clinical picture and communicate effectively with laboratory staff about what further work to do on patient isolates. Although you will not be expected to process specimens as a consultant, it is very important that, as a trainee, you spend time in the microbiology laboratory to gain an understanding of the way the laboratory works. You will do more of this in early part of your training than later on.
You will get involved in the management of outbreaks within the hospitals such as during the COVID pandemic, perhaps dealing with an increased number of wound infections from the cardiac surgical unit or of diarrhoea and vomiting on an elderly care ward for example. As you get more senior, you may end up leading root cause analysis investigations to determine the cause of a patient’s hospital-acquired infection and make recommendations about how to reduce the risk of that event happening in future. Many people will seek your advice about things that you have never had to deal with previously in your medical career: “are silver-impregnated urinary catheters better than non-silver impregnated ones?”, and “someone’s baby was given the wrong breast milk from the breast milk bank, what should we do?'' are just some of the examples. You will become adept at searching literature and make pragmatic decisions based on your increasing knowledge and experience. You may get the opportunity to evaluate new diagnostic tests and laboratory equipment – perhaps presenting your findings regionally, nationally or internationally. Quality assurance and audit is an important part of being a microbiologist, as with all medical specialties.
What personal qualities are desirable for the microbiology part of my job?
You must be able to interact effectively with everyone from hospital cleaners, junior medical staff and laboratory technical staff to senior surgeons, GPs and hospital management. Infection Prevention and Control for example is as much about understanding human behaviour and hospital politics as it is about the science of decontamination and organism biology. You will need persistence and patience if you want to bring about cultural change, perhaps in a unit that overuses antibiotics for example.
You should have an eye for detail and avoid jumping to conclusions; however obvious things may be at first glance, infectious diseases and patients do not read text books! Clarity of thought and expression are essential.
What else should I know about the training?
ID/microbiology and ID/virology have an extra examination (FRCPath part 2) compared to ID/GIM in order to meet the training requirements of the laboratory specialties.. Research during training is encouraged and some trainees go on to complete higher research degrees.,. Diplomacy is an essential skill, because of the multiple interactions with other teams. The specialty is competitive and attracts high caliber trainees. You may need to move region to get a training post (so too for consultant posts).
On call
All rotas across region meet the contractual requirements for junior doctors..
On call rotas and corresponding pay supplements vary across the training years depending on the training programme (ID-GIM or ID-MM/MV). ID/GIM programmes have on call medicine throughout. ID-MM/MV programmes may have periods without on call but this is variable. MM/MV rotas are normally an overnight on-call rota for phone advice, with weekend daytimes on-site
All infection trainees undertake general acute medicine on call during CIT. Separate ID on-call is also done at Heartlands hospital (early evening and weekend daytime only), with a commensurate reduction in the GIM on-call frequency. We value some ongoing training in acute general medicine for all ID-micro trainees, particularly in the first year, given that most ID units do not have separate out of hours on-takes for emergencies, and also recognising the need for a good working knowledge of acute admissions units for all physician infection specialists.
What does a long term Career in Infection Offer?
Huge variety! There is virtually no private medicine. Traditionally, many consultants’ posts have a strong academic component. The recent trend is for more full time clinical posts and many post are now advertised as Clinical Infection Specialist posts.ID/GIM trained consultants have also been sought after for jobs which include acute or general medicine. This variety of opportunities means there is very little concern about lack of consultant posts for infection specialists at the end of training.
How do I make myself competitive for training posts?
Commitment to the specialties needs to be demonstrated, particularly for ID-GIM, for example by tropical electives, a self funded DTM&H, etc.
|
How can my Career be Further Developed?
Out of Programme (OOP) Experience or Research is strongly encouraged and well supported for our trainees by the Deanery, and all recent trainees have spent or are embarking on extended periods of time in research or further studies, mostly in overseas, including resource-poor settings
Examples of OOP placements:
- Sierra Leone Ebola Treatment centres
- MRC funded studies in Guinea Bissau on trachoma
- Welcome Trust units in SE Asia studying severe malaria, and melioidosis as a model of sepsis
- Welcome Trust funded study of Cryptococcosis& immune reconstitution in HIV in South Africa
- Assessment of training needs for HIV care in Henan Province China
- Epidemiology of Tuberculosis, Warwick
- Rotavirus studies, Vaccine research group, Oxford
Other trainees have had time out of programme to do a Master’s in Public Health (in Sydney) and a Master in Medical Education
We regularly have Birmingham University Medical students from year 3-5 attached to the ID department at BHH. Trainees get involved with bedside teaching, as well as formal teaching sessions at both the University of Birmingham and the University of Warwick.
ROTATIONS
Please note that rotations will be designed to allow the curriculum competencies to be achieved and will include placement at a number of training sites over the 5 years of training.. We make every effort to avoid successive placements of any individual at hospitals at opposite poles of our geographical region and also to take personal circumstances into account when finalising rotations. Given the complexity of the ID-GIM-MM/MV training programmes, however, as well as the movement of many trainees in& out of programme, we cannot guarantee specific rotation patterns more than 4 months before the main August rotation date.
Out of Programme (OOP) time
There are many reasons why a trainee may go out of programme. Some of the main reasons are;
- Time out for research or further studies
- Personal and/or family reasons
* OOP may be at any point after first and before final year. It often extends for 3yrs (occasionally more) Up to one year can theoretically count towards training though increasingly trainees are choosing not to request this accreditation because of overall shortened length of training.
|
|